A Cautionary Tale About Deep Vein Thrombosis
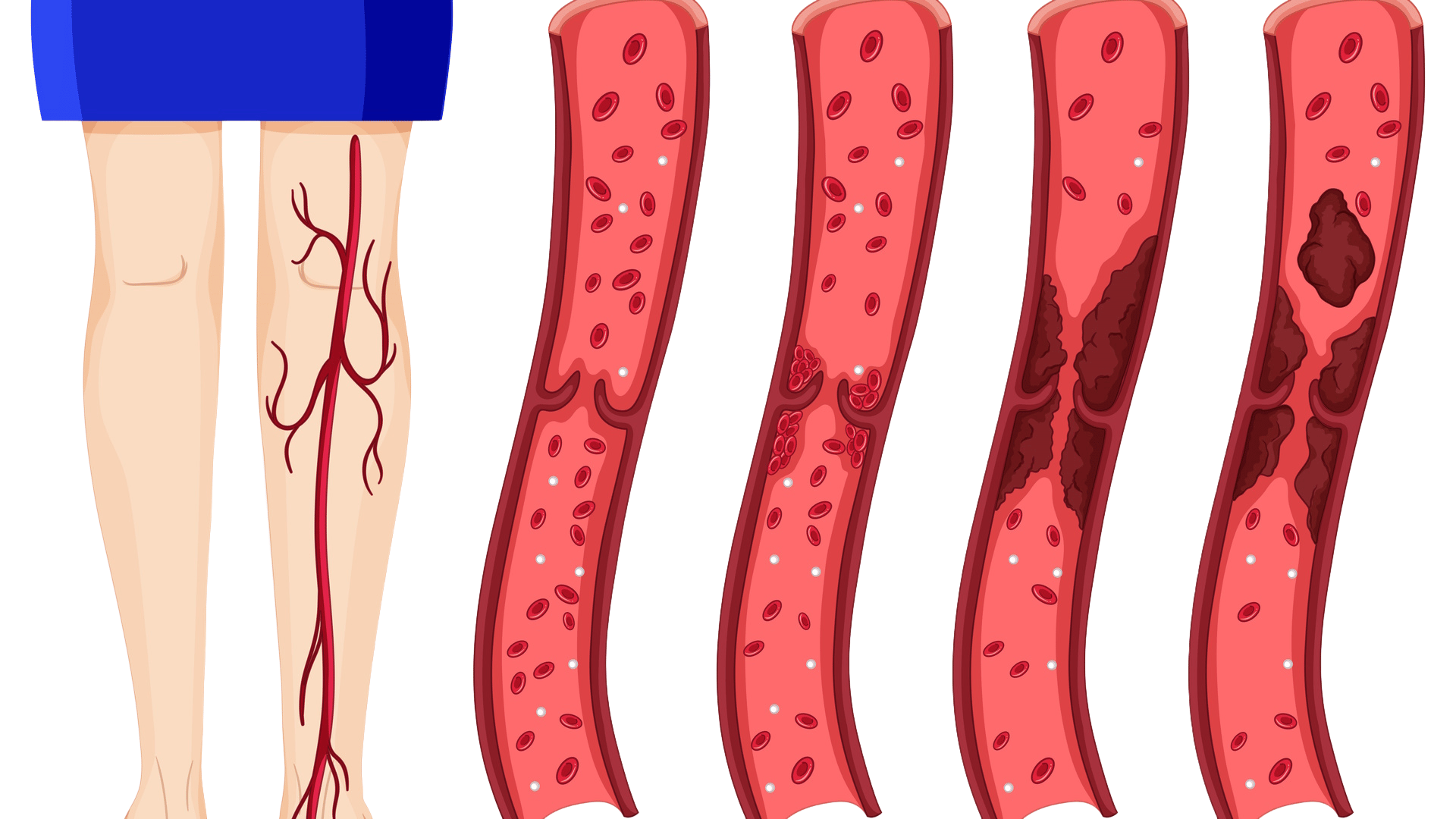
Mr Sharma’s Close Call: Understanding Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE) A Normal Evening Turns into a Medical Emergency Mr. Sharma, a 50-year-old shopkeeper, was wrapping up his day, counting his earnings, when he suddenly felt a sharp chest pain, along with shortness of breath and profuse sweating. Alarmed, his wife and daughter rushed him to the nearest hospital. At the hospital, Dr. Nita diagnosed him with a pulmonary embolism (PE)—a life-threatening condition caused by a blockage in the arteries of the lungs. The Hidden Danger: Deep Vein Thrombosis (DVT) Mr Sharma was confused. “But I don’t smoke or drink (too much), how did this even happen?” Dr. Nita gently explained,“You’ve been sitting for long hours without moving much. This caused deep vein thrombosis (DVT)—a condition where blood clots form in deep veins, usually in the legs. One of these clots broke free, travelled to your lungs, and blocked a pulmonary artery. That’s what caused your chest pain and breathlessness.” What is Deep Vein Thrombosis (DVT)? DVT is a medical condition where blood clots form in deep veins, often in the legs. If left untreated, these clots can travel to the lungs, causing pulmonary embolism (PE), which can be fatal. Who is at Risk of DVT and PE? People over 40 years of age Those with sedentary lifestyles (desk jobs, long travels, shopkeepers) Post-surgery patients Pregnant women People with chronic illnesses Individuals with increased estrogen levels (e.g., on birth control pills) About 30% of people who experience DVT or PE are at risk of recurrence, making awareness and prevention crucial. Symptoms to Watch For: Deep Vein Thrombosis (DVT): Swelling in one leg (often below the knee) Redness or warmth Pain or tenderness in the leg Pulmonary Embolism (PE): Sudden chest pain Shortness of breath Rapid heartbeat Coughing (sometimes with blood) Preventing DVT and Pulmonary Embolism Dr. Nita advised Mr Sharma—and his family—on how to prevent another episode: Top Tips to Prevent DVT and PE: Move Every Hour – Especially during long hours of sitting or standing. Avoid Sitting Cross-Legged – Reduces blood flow in the legs. Stay Hydrated – Helps maintain healthy blood viscosity. Maintain a Healthy Weight – Reduces pressure on veins. Exercise Regularly – Even a daily walk improves circulation. Wear Compression Stockings – If recommended by a doctor. Why Awareness Matters Deep vein thrombosis is underdiagnosed but entirely preventable. If you or someone you know experiences unexplained leg swelling or chest pain, seek immediate medical help. A simple lifestyle change—like standing up once every hour—can literally save your life. Final Thoughts Mr Sharma’s story is a powerful reminder that even non-smokers and non-drinkers can suffer from conditions like DVT and PE due to inactivity. A few proactive steps can keep your blood flowing—and your life going.